Best Treatment For Acute Pericarditis Disease
Overview
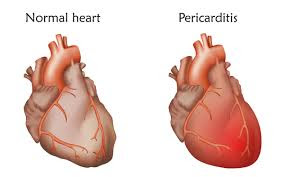
An inflammation of the pericardium, the thin sac that surrounds the heart, is known as acute pericarditis. While it can be uncomfortable, the good news is that most cases are self-limiting and resolved without significant complications.
What triggers acute pericarditis?
Viral and bacterial infections:
- Viral infections, such as the flu or Covid-19, are common culprits.
- Bacterial infections, including tuberculosis, can also lead to pericarditis.
Inflammatory Conditions:
- Chronic autoimmune conditions like rheumatoid arthritis and lupus may trigger pericarditis.
- Sometimes, pericarditis occurs alongside myocarditis (inflammation of the heart muscle), known as myopericarditis
Thyroid Disorders:
- Abnormalities in thyroid function can contribute to pericardial inflammation.
Chest Injury:
- Trauma to the chest, such as knife or bullet wounds, can cause acute pericarditis.
- Inflammation After Heart Surgery:
- Surgical procedures involving the heart can sometimes lead to pericardial inflammation.
Other Rare Causes:
- Radiation therapy to the chest (e.g., for lung cancer) or, very rarely, cancer itself can be implicated.
- Certain medications (e.g., phenytoin, warfarin, heparin, and procainamide) may also play a role.
- Interestingly, in some cases, the cause remains elusive, and we label it as idiopathic pericarditis—frustrating.
Symptoms
Typically include:
- Sudden, sharp chest pain that may spread to the shoulders, neck, or back
- Pain that's worse when lying down or breathing deeply and less severe when sitting up
- Pain that worsens when coughing, swallowing, or taking a deep breath
- A dry cough
- Palpitations: the sensation that your heart is pounding rapidly or erratically
- Anxiety or fatigue
- The Fever
- Swelling of your legs, feet, and ankles in severe cases
Symptomatic Treatment:
- If laboratory results confirm the clinical diagnosis, symptomatic treatment should start.
- The most prevalent are aspirin and NSAIDs, or non-steroidal anti-inflammatory medicines. These are useful for reducing swelling and pain.
- We advise initial treatment with colchicine and aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). Recurrences are less likely, and symptoms may be less severe as a result. We may try low-dose corticosteroids when other options, such as aspirin/NSAIDs and colchicine, are not available or do not work, or when we suspect an autoimmune condition.
Considerations for risk and outlook:
- Tamponade, a useful method for stopping bleeding, recurrences, and constriction are all signs that there will be more problems during follow-up.
- A bad prognosis is likely if the fever is high, the illness lasts for a long time, there is a lot of fluid around the heart, the heart stops beating, or the patient doesn't get better after seven days of taking nonsteroidal anti-inflammatory drugs (NSAIDs).
- Experts agree that immunodeficiency, trauma, anticoagulant treatment, and myopericarditis are minor risk factors.
- If there is a serious underlying issue or relevant risk factors, it is necessary to admit the patient to the hospital and do additional investigations.
Watching and Following Up:
- Serum C-reactive protein levels guide treatment duration and response.
- Patients who do not exhibit symptoms of systemic inflammatory disease can receive treatment as outpatients with the use of empiric anti-inflammatory medicine and brief follow-up.
- Treatment should be individualized based on the underlying disease if a cause other than viral infection is found.
How can we identify acute pericarditis?
Assessment in the Clinic:
Assessing the Body: A typical discovery is the characteristic pericardial friction rub, which occurs when the inflamed pericardium rubs against the interior of the chest wall. Your heart seems to be pounding out an unpleasant tune.
Warning Signs: When making a diagnosis, it is important to consider your medical history as well as any risk factors, such as a history of infections, autoimmune diseases, or recent heart surgery.
Evaluation Standards:
- Two of the four criteria for acute pericarditis can be satisfied:
- The characteristic ache in the chest: That sudden, stabbing ache in the chest that I described before.
- A pericardial friction rub is the scratchy sound you hear during the physical exam.
- Alterations to an electrocardiogram (ECG) include a new, broad, upward-curving ST elevation or a PR depression.
- The presence of new or worsening fluid surrounding the heart as seen by echocardiography is known as pericardial effusion.
- It is common for blood tests such as serum troponin and C-reactive protein (CRP) to show signs of systemic inflammation.
Additional Investigations:
- ECG: detects electrical activity changes associated with pericarditis.
- Pericardiocentesis: If cardiac tamponade (life-threatening fluid accumulation) is suspected, urgent drainage is necessary.
- Other blood tests, including serum urea and electrolytes, full blood count, and liver function tests, may provide further insights.
Pericarditis treatment guidelines
- Symptomatic Treatment:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These are typically the first-line treatments. They help reduce inflammation and alleviate pain. Common NSAIDs include aspirin or other NSAIDs like ibuprofen.
- Colchicine: This medication is recommended as an adjunct to NSAIDs. It helps prevent recurrences and may shorten the duration of symptoms. Typically, patients receive colchicine for approximately three months.
- Gastroprotection: If you’re taking NSAIDs, consider using a proton pump inhibitor (PPI) or H2 blocker to protect your stomach lining.
- Corticosteroids:
- Low-dose corticosteroids may be considered in specific situations:
- When there are contraindications or failure of aspirin/NSAIDs and colchicine.
- When an infectious cause has been excluded.
- When there’s a specific indication (e.g., autoimmune disease)
Monitoring and Follow-up:
- Serum CRP (C-reactive protein) levels guide treatment duration and response.
- If you don’t have signs of systemic inflammatory disease, you can manage acute pericarditis as an outpatient with empiric anti-inflammatory medications. Follow up after about a week to assess treatment response.
- If an alternative cause (other than viral infection) is identified, specific therapy should be tailored to the underlying disorder.
Lifestyle Considerations:
- Rest: Give your heart some downtime. Avoid strenuous activity during acute pericarditis.
- Positioning: Leaning forward often alleviates chest discomfort, so find a comfy position.
- Hydration: Stay well-hydrated—it’s beneficial for your overall health and might help ease symptoms.
How can I prevent pericarditis recurrences?
Tell me more about colchicine treatment.
- What is gout? Gout is a type of arthritis caused by the buildup of uric acid crystals in the joints. It leads to intense pain, redness, swelling, and heat in the affected joint.
- How Colchicine Helps: Colchicine prevents and treats gout attacks. It doesn’t cure gout, but it significantly reduces inflammation during acute attacks. By decreasing inflammation, it eases the pain and discomfort associated with gouty arthritis.
Familial Mediterranean Fever (FMF):
- Colchicine is also used to treat FMF, a rare inherited disorder characterized by recurrent episodes of fever, abdominal pain, and inflammation. FMF primarily affects people of Mediterranean descent.
- In FMF, colchicine helps prevent and reduce the frequency of these episodes by suppressing inflammation.
Conclusion
Early diagnosis and treatment are crucial. If you experience symptoms like chest pain, fever, or shortness of breath, don’t hesitate to seek medical attention. Individual cases can vary, and your doctor will tailor treatment based on your specific situation.
No comments:
Post a Comment