Lack of sleep can disrupt your weight loss goals
Info
While food and exercise are vital to weight loss, sleep is as important. Lack of sleep can disrupt your diet and exercise habits, among other reasons. If you've ever slept poorly and craved chips and sweets the next day, you've seen this.
"There is no question that good quality and sufficient duration of sleep are beneficial to reaching or maintaining a healthy weight," says Hackensack Meridian School of Medicine sleep medicine specialist Peter Polos, MD, PhD, associate professor of internal medicine in Nutley, New Jersey.
Learn why the body reacts that way and how to optimize your sleep to reach your weight goals.
Sleep and Weight Loss
Not getting enough sleep can affect weight loss or growth in various ways.
It Disbalances You
- "Getting too little sleep contributes to weight gain by upsetting the balance between how much we eat and how much fuel we burn," explains Kaiser Permanente Honolulu pulmonologist and sleep medicine expert Shanon Makekau, MD.
- A two-week sleep extension intervention reduced daily energy consumption by 270 calories in 80 overweight people who slept fewer than 6.5 hours each night. The individuals expended the same amount of energy daily, creating a negative energy balance that can cause weight loss. It May Increase Hunger the Next Day
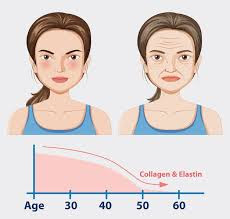
- Ghrelin, which makes you hungry, and leptin, which keeps you full, may rise in sleep-deprived people. "This can result in increased appetite, and hence weight gain," Polos explains.
More Time to Eat
Dr. Makekau thinks less sleep means more time to eat.
You snack more
- Unfortunately, sleep-deprived people often eat unhealthy meals like donuts and fried food. "Sleep-deprived individuals tend to eat foods with greater amounts of carbohydrates and calories," Polos adds.
- One narrative review found that disturbed sleeping patterns increase energy (calorie) intake, mostly from snacking on high-fat and high-carb foods.
- Sleeping more can lead to healthier food choices. "Getting enough good-quality sleep supports daytime energy, mood, concentration, and motivation," he explains. "All of these factors play an important role in making good choices during the daytime."
You Move Less When Tired
"People who don't get enough sleep are more sedentary and are less likely to engage in moderate to vigorous activities such as sports or exercise," he adds. Consider the last time you slept five or six hours. You probably battled to get through the day and weren't eager to work out.
Scientific Evidence on Sleep and Weight Loss.
The video explains how sleep affect weight loss
Sleeping too little or too much has been linked to weight gain or loss in many studies.
A cross-sectional study of 2,500 participants indicated that sleeping fewer than seven hours doubled the risk of overweight and obesity compared to sleeping seven to nine hours. Another observational study of 125 overweight or obese adults indicated that better sleep health increased weight and fat loss.
Sleep and weight loss are surprisingly interconnected.
Here are some fascinating facts:
- Hormonal Balance: Sleep affects hormones like leptin and ghrelin, which regulate appetite. Poor sleep can increase ghrelin (a hunger hormone) and decrease leptin (a satiety hormone), leading to overeating.
- Food Choices: Sleep deprivation can make you crave high-calorie, sugary foods. It may also reduce your energy for preparing healthy meals.
- Metabolism: Lack of sleep can slow down your metabolism, making it harder to burn calories.
- Physical Activity: Feeling tired due to insufficient sleep can reduce your motivation to exercise, impacting weight management.
It's fascinating how something as simple as sleep can play such a crucial role in maintaining a healthy weight.
Explain how leptin and ghrelin impact weight.
Leptin and ghrelin are two key hormones that play significant roles in regulating appetite and weight:
Leptin:
Often called the "satiety hormone," leptin is produced by fat cells and signals your brain when you have enough energy stored. Essentially, it tells your brain that you're full and don't need to eat. If leptin levels are low or the brain becomes resistant to its signal (as can happen with chronic overeating or obesity), you may feel hungry more often, even if your body has plenty of stored energy.
Ghrelin:
Known as the "hunger hormone," ghrelin is produced in the stomach and signals your brain to stimulate appetite. Its levels rise before meals, making you feel hungry, and drop after eating. When you don't get enough sleep, ghrelin levels tend to increase, leading to a heightened sense of hunger.
Together, these hormones create a balance: leptin suppresses appetite, while ghrelin stimulates it. Disruptions in this balance, such as poor sleep, chronic stress, or unhealthy eating habits, can lead to overeating and weight gain.
How do diet and exercise influence leptin and ghrelin levels?
Diet and exercise play a significant role in regulating leptin and ghrelin levels, which in turn impact hunger and weight management:
Diet:
Caloric Intake: Extremely low-calorie diets can lower leptin levels and increase ghrelin, leading to heightened hunger and reduced satiety. A balanced diet helps maintain healthier levels of these hormones.
Nutrient Quality: Diets rich in whole foods, fiber, and healthy fats can support better hormonal balance, reducing ghrelin spikes and promoting leptin sensitivity.
Exercise:
- Leptin Sensitivity: Regular physical activity, especially high-intensity exercise, can improve leptin sensitivity, helping the brain respond more effectively to leptin's satiety signals.
- Ghrelin Regulation: Exercise can temporarily suppress ghrelin levels, reducing hunger post-workout. However, the effect may vary depending on the intensity and duration of the exercise.
By combining a nutritious diet with consistent exercise, you can create a positive impact on these hormones, supporting better appetite control and weight management.
What specific diets can help regulate leptin and ghrelin?
Certain dietary choices can help regulate leptin and ghrelin levels, promoting better appetite control and weight management:
- Nutrient-Dense Foods: Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats. These foods provide essential nutrients and help maintain hormonal balance.
- High-Fiber Diet: Fiber-rich foods like legumes, oats, and leafy greens can promote satiety and stabilize ghrelin levels.
- Protein-Rich Meals: Including protein in your meals can suppress ghrelin and enhance leptin sensitivity.
- Healthy Fats: Omega-3 fatty acids found in fish, nuts, and seeds can improve leptin sensitivity.
- Avoid Processed Foods: Processed and sugary foods can disrupt hormonal balance and lead to leptin resistance.
By incorporating these dietary habits, you can support a healthier hormonal balance.
What are examples of nutrient-dense meals?
Here are some examples of nutrient-dense meals that are both delicious and packed with essential nutrients:
Superfood Salmon Salad: A mix of salmon (rich in omega-3 fatty acids), leafy greens, cherry tomatoes, avocado, and a light vinaigrette dressing.
Vegetable Curry: A vibrant curry made with a variety of vegetables like bell peppers, carrots, and spinach, cooked in coconut milk with aromatic spices.
Mediterranean Quinoa Bowl: Quinoa topped with grilled chicken, cucumbers, olives, cherry tomatoes, and a drizzle of olive oil and lemon juice.
Garden Veggie Frittata: Eggs mixed with spinach, mushrooms, and bell peppers, baked to perfection for a protein-packed breakfast or brunch.
Lentil and Sweet Potato Stew: A hearty stew with lentils, sweet potatoes, carrots, and a touch of cumin and paprika for flavor.
These meals are not only nutrient-dense but also versatile—you can easily adapt them to suit your preferences.
Tips for Quality Sleep During Weight Loss
Here are some tips to improve sleep quality while supporting weight loss:
Stick to a Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends, to regulate your body's internal clock.
Create a Relaxing Bedtime Routine: Engage in calming activities like reading, meditation, or taking a warm bath before bed.
Limit Screen Time: Avoid screens (phones, tablets, TVs) at least an hour before bedtime, as blue light can interfere with melatonin production.
Optimize Your Sleep Environment: Keep your bedroom dark, quiet, and cool. Consider blackout curtains, white noise machines, or a fan.
Watch Your Diet: Avoid heavy meals, caffeine, and alcohol close to bedtime, as they can disrupt sleep.
Exercise Regularly: Physical activity can improve sleep quality, but try to finish intense workouts at least a few hours before bed.
Manage Stress: Practice relaxation techniques like deep breathing or yoga to reduce anxiety and promote better sleep.
These habits can help you achieve restful sleep, which is essential for regulating hunger hormones and supporting weight loss.
Does Sleep Increase Metabolism?
Sleep plays a crucial role in regulating metabolism. During sleep, your body undergoes processes that support metabolic health, such as repairing cells, balancing hormones, and managing energy use. Poor sleep quality or insufficient sleep can disrupt these processes, leading to issues like insulin resistance, slower metabolism, and weight gain.
Interestingly, while you burn fewer calories during sleep compared to being awake, quality sleep can help maintain a healthy metabolism and support weight management
Can Lack of Sleep Increase Appetite?
Lack of sleep can increase appetite. Sleep deprivation disrupts the balance of hunger-regulating hormones, ghrelin and leptin. Ghrelin, the "hunger hormone," rises with insufficient sleep, making you feel hungrier. Meanwhile, leptin, the "satiety hormone," decreases, reducing the feeling of fullness.
Additionally, sleep deprivation can lead to cravings for high-calorie, sugary foods and impair decision-making, making it harder to resist unhealthy options.
5 Tips for Better Sleep When You're Trying to Lose Weight
Here are some tips that can help you snooze more and avoid packing on pounds.
Exercise for at least 20 minutes every day. Working out daily can promote energy usage in the body and increase body temperature, which in turn can help you sleep soundly at night.
Just don't exercise too close to bedtime, or it could backfire and make it tough to settle down.
Eat well. Certain foods promote sleep, including walnuts, almonds, turkey, and fatty fish, says Kristin Gillespie, RD, a contributor for Exercise With Style based in Virginia Beach, Virginia. Spicy and fatty foods can have the opposite effect, she says.
Keep your bedroom dark. Being exposed to artificial light while sleeping, such as from TV, devices, or a bedside lamp, is associated with an increased risk of weight gain and obesity.
Avoid eating right before bedtime. One small crossover trial found that late eating increases wake-time hunger, decreases wake-time energy expenditure and leptin (which makes you feel full), and may favor increased fat storage and obesity risk.
Go to bed early. Adults who are chronically sleep deprived and go to bed late may be more likely to gain weight due to greater daily caloric intake and consuming calories later in the evening.
Conclusion
Sleeping too little can cause you to eat more, which can lead to weight gain, while sleeping more can cause you to reduce your caloric intake, promoting weight loss.
Sleep deprivation may lead to increased levels of the neurotransmitter ghrelin, which makes you feel hungry, and lower levels of leptin, which makes you feel full.
Disturbed sleeping patterns have been shown to lead to an increase in calorie intake, mainly from snacking, especially on foods rich in fat and carbohydrates.
Getting better sleep can help you avoid weight gain and also give you more energy during the day to exercise and make healthier food choices.